This is Part 2 of my Laparoscopic Hysterectomy journey. If you haven’t already, please read Part 1 to understand the background of my condition and surgery.
Let’s get to part 2.
Details of my procedure
I had a total of 4 weeks to prepare for the surgery and I had just a couple of things to do. 1. complete forms for the hospital and anaesthetist. 2. get prior approval from my health insurance company. 3. do a blood test 2 weeks before my surgery date. I have been scheduled for surgery on 31st July at Ormiston Hospital and was booked in for 2-3 days of hospital stay (depending on how I recover, I could leave earlier). The hospital is close to home and had a nice little cafe downstairs for visitors. The full name of the procedure is: “Complex Total Laparoscopic Hysterectomy and Bilateral Salpingectomies” – remove of the uterus, fallopian tubes, and cervix only. Leaving the ovaries. This is proposed to be done via 3 keyhole incisions instead of a caesarean. The uterus will be removed in small pieces through the vagina. In case of complications, I have approved the surgeon to do a caesarean. I am also not keeping the removed tissues.

Estimated cost of my procedure
Leading up to the day of the procedure
A week before my procedure, I started packing my hospital bag. This is the first time I have had a planned stay at the hospital and even when I gave birth, I was only at the hospital/birthing unit for maximum 2 nights. (I packed a bunch of items, but I will spare you the details and just list out the items I ACTUALLY USED. A set of comfortable, loose PJs, a pair of knickers, chargers and cables, essential skincare, lip balm, headband (to keep my hair away), toothbrush and toothpaste and disposable face towels). I wore the same set of clothes I wore to the hospital when I left. I did not bring socks and slippers because I was provided compression socks and grippy socks from the hospital anyway. There were basic toiletries like body soap, shampoo and conditioner as well as a hair dryer.)
I started taking Kiwicrush daily – liquid Kiwifruit to help with constipation. I do not usually suffer from constipation (even though I have been taking iron supplements on a daily basis), but I would like my bowels to have as little “content” as possible. I have also prepared waterproof dressings and silicone tape for scar healing further down my recovery route. I also had my hair cut 2 weeks before my procedure so I don’t need to worry about getting it done during my recovery.

The Friday before my surgery, I received a call from the hospital to let me know about the details. We double-checked our surgery details – what procedure we will be doing, and our scheduled time. I was asked to not eat anything 6 hours before surgery, and I was only allowed plain water 2 hours before the surgery. I should bring any medication that I have (inhaler), bring personal toiletries like toothbrushes, toothpaste, skincare, etc. There will be towels and flannels in my private ensuite room. I would be wearing hospital gowns for most of the time until I feel good enough to change into my own pyjamas. There will be free wifi, Sky TV, etc. during my 4-day stay. I should wear loose clothing and a mask when I arrived.
My husband would accompany me to the hospital and surgery should start in about an hour from my time of arrival and the surgery should take around 2.5 hours. Recovery would be around 1 hour. So my husband could call the hospital to check what I was doing around 3.5-4 hours after I go into the theatre. I am scheduled to go in at 12:30 pm, so once I am finished, it would be close to dinner time for my family anyway.

Day of the surgery
My surgery was scheduled for 12:30 pm Monday and I received a phone call from the Hospital to ask me to come in earlier at 12 noon because the name on my blood test was incorrect. I had no food in the morning, and nothing to drink after 10 am as well. We arrived and were swiftly taken by the nurse to do some account checks and tests. We did a quick weight and height check, a RAT test, a pregnancy test, and blood pressure checks. I was 154/100 because I was getting really nervous.
After getting changed into paper underwear, a hospital blue gown and a thin waffle robe for warmth and cover. I was also given compression socks to wear and grippy socks to keep me from slipping. I was given some paracetamol to take before the anaesthetist put an IV on the back of my left hand and drew blood from me for a blood test. Usually, IV is inserted just prior to surgery, so having this inserted 30mins before my surgery elevated my anxiety quite a lot and it was also a little sore.

A physiotherapist also sat down to talk to us briefly about post-surgery recovery. She gave me a spirometer for my deep breathing exercise and I was expected to try using it 10 times an hour. Pre-surgery me: 5 and I was already feeling a little light-headed. Let’s just say post-surgery, I hated this thing.

spirometer
We waited in the waiting area and watched doctors and nurses pass us for around 45 mins. Then I was greeted by the anaesthetist technician for further checks and to let me know the theatre is ready for me. My husband and I hugged and said goodbyes and I walked into theatre 2 to see the stark white interiors and people bustling around. There were at least 5 people including my surgeon in the theatre and I climbed onto the bed and lay down with my arms spread open. People were working on me immediately. Inserting an IV line, attaching monitors to my body and giving me an oxygen gas mask.
I was asked my name, date of birth and what procedure I will be getting. I mistakenly said I was having a hysteroscopy! About a minute went by, I was told to close my eyes and just relax. I noticed a weird smell in the oxygen mask and a light sting in my IV and within a few seconds, I was completely out.
After the surgery
When I opened up my eyes I was already in the recovery area linked to beeping machines and a blood pressure device attached to my right arm. As soon as I opened my eyes, a nurse sitting next to me said something and I replied, but I completely forgot what we said. I was out again. I was feeling really drowsy and a little nauseous. The next time I was conscious, I was being wheeled away from the recovery area and down to level 2 via the lift and into my private ensuite room.
I was in and out of consciousness for not sure how long, but the nurses were constantly around to make sure I am OK. My temperature and blood pressure were checked every 20 minutes, then hourly. I also had an IV line and I had no idea what it was feeding me. I also had this uber-annoying thing around my calves that inflates and deflates with rhythm to keep the blood in my legs from clotting.


My mid-section was painful, and I could only take short breaths. I was also feeling pain on my shoulders which I was told is the side-effects of the gas they had to fill my tummy up with and it will go away soon. I fell asleep again until my entire family stepped in the door (husband, kids and my mother-in-law). I immediately asked for the time and it was 7:30 pm (there were no clocks in the room). I tried my best to stay awake while they were here and I think my body was ready for another nap after 30 mins and I was talking to them with my eyes closed.

After my family left, I asked for my dinner because I was famished (I declined the first time they asked if I wanted to eat)! Dinner came and I could only down a few sips of soup and a couple of bites of bread. I drank the glass of apple juice, but I was unable to even eat the apple crumble and ice cream (cry!). I fell asleep with the table still in front of me and the tray of food was eventually taken away.
For the first night, I was alternating between the medication (pain, nausea and to assist bowel movement), blood pressure checks and temperature checks. At around 11 pm, I was asked if I wanted to go and have a walk around the ward. Initially, I declined, but the nurse said it is highly suggested that patients start walking on the first night to speed up recovery, release gas, assist in bowel movements, prevent blood clots, etc. So I ended up saying yes for a walk. I did not feel light-headed, but I could feel moderate pain in my abdomen.

Day 1 dinner
At midnight, I was so hungry I asked for cheese and crackers which went down very well. Sleep was not very good for the first night mostly because of that super annoying leg thingy and the dripping IV noise. My husband connected my phone to my charger and put it next to me so I was able to check the time. I was waking up hourly until the next day.

Day 1 night snack
Second-day post-surgery
Nothing much changed, after midnight, they were monitoring me every 4 hours and by morning, they were monitoring me every 6 hours, leaving me plenty of time to rest. They have also taken the catheter out in the morning as well as the device on my legs. I was able to eat my breakfast, which was a ham, egg and cheese omelette with a side of toast and apple juice (I couldn’t finish the omelette). My husband came to accompany me after dropping the kids off and he was able to do some work on his laptop in the room. Watching the TV, and playing games on my phone. I was able to get in and out of my bed without assistance. Just before my husband left, I had a chicken and cheese toastie with fruit salad and honey and ginger tea. Toastie was good, but I couldn’t finish.

Day 2 breakfast – ham and cheese omelette

Day 2 lunch – chicken and cheese toastie
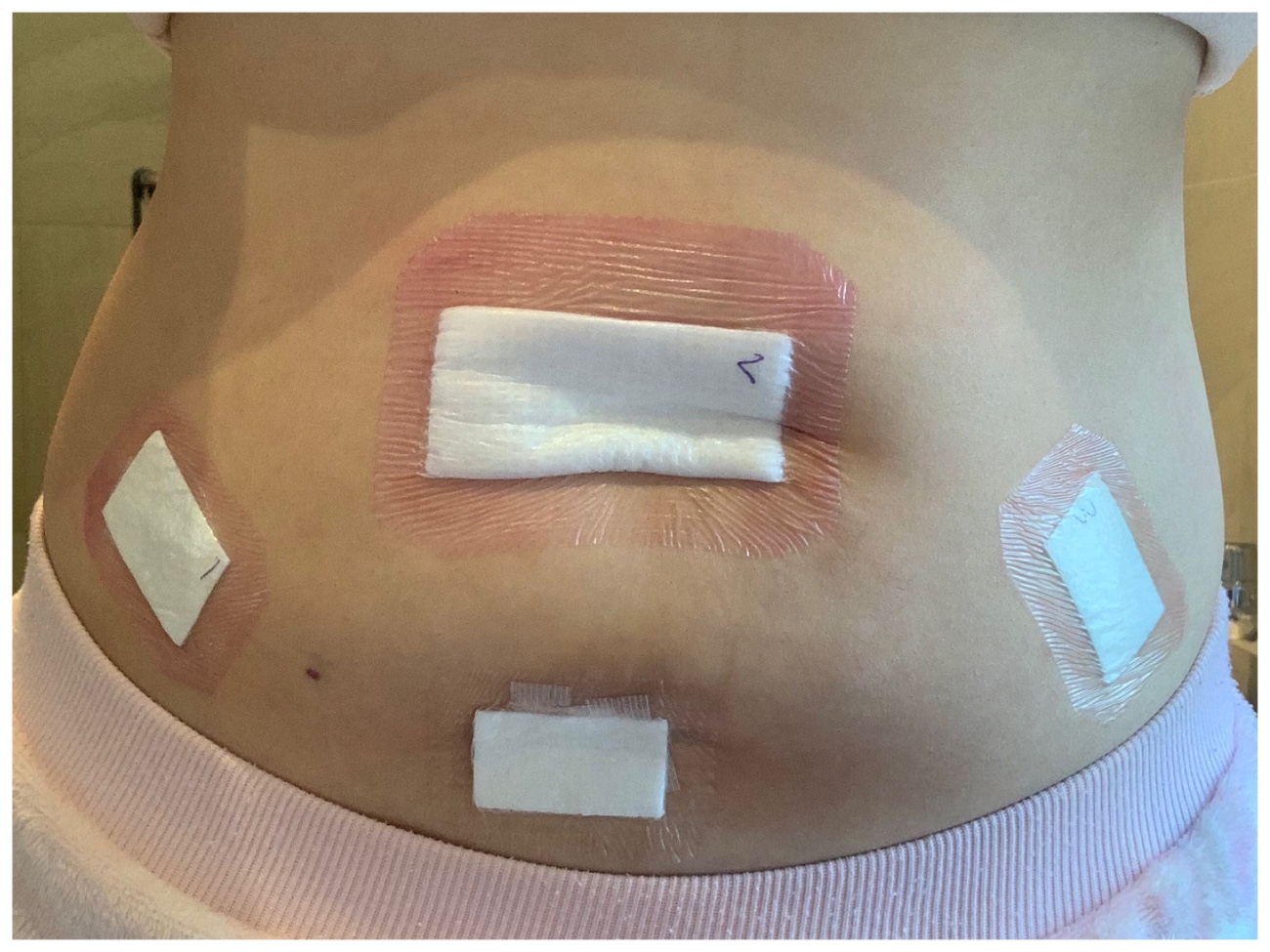
My surgeon (gynaecologist specialist) came to visit me and talked to me about my surgery and went through the pictures with me. I had a total of 4 incisions – 3 for the laparoscopic procedure and one larger one to remove my uterus + fibroid. My fibroid measured 7.5m wide in total so it was bigger than expected.

surgery photos – fibroid

surgery photos – fibroid

surgery photos – fibroid removed, stitches in place
After my surgeon left, my parents came to visit with homemade soup, chicken wings and cut-up apples. I immediately had an appetite for apples and drank some soup. They stayed for half an hour and left. Then the physiotherapist came to talk me through in-bed exercises and I had to practice on the spirometer. I could only get one ball up at that time.
Come night time, I was served dinner at 6 pm and I picked pulled pork with roasted veggies, creme brulee and also apple juice. I also could not finish the main but finished the apple juice and creme brulee.

Day 2 dinner – pulled pork and roasted veggies. Creme brulee
Throughout the day, my pain level was very well managed, nothing over 3 and I was able to get out and about, brush my teeth and wash my face. Nurses were commenting that I should be able to leave very soon. A part of me wanted to stay longer because of all the peace and quiet, plus the adjustable bed. But another part of me wanted to go because I didn’t really like the food and I missed my family, plus I’m a bit bored.
Below are just some of the photos of my private ensuite room. They clean the bathroom on a daily basis, and change sheets on a daily basis as well.

Private ensuite room

Private ensuite room

Private ensuite room

Toiletries

Hospital care pack
On the morning of the 3rd day, I met with the physiotherapist to go through the simple exercises I need to do at home to assist with recovery. I also had a bowel movement about an hour before I was discharged. My surgeon came to check up on me and run me down the medications she has prescribed to me. At around 11 am, I was discharged and we picked up my medication from the pharmacy downstairs and went home.
As I am writing this, I am already 9 days post-op. I am walking, doing light housework, eating well, with very minimal pain and no digestive issues. I should be back to work in a few more days but just won’t be driving for another 2 weeks. I will update again in Part 3!
Recovery and life after surgery are to be continued in Part 3…